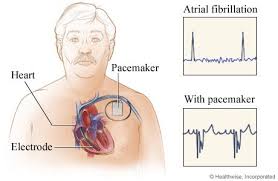
A pacemaker (or artificial pacemaker, so as not to be confused with the heart's natural pacemaker) is a medical device which uses electrical impulses, delivered by electrodes contracting the heart muscles, to regulate the beating of the heart.
The primary purpose of a pacemaker is to maintain an adequate heart rate, either because the heart's natural pacemaker is not fast enough, or because there is a block in the heart's electrical conduction system. Modern pacemakers are externally programmable and allow a cardiologist to select the optimum pacing modes for individual patients. Some combine a pacemaker and defibrillator in a single implantable device. Others have multiple electrodes stimulating differing positions within the heart to improve synchronisation of the lower chambers (ventricles) of the heart.Pacemaker facts*
- A pacemaker is a small device that's placed in the
chest or abdomen to help control abnormal heart rhythms. This device uses
low-energy electrical pulses to prompt the heart to beat at a normal rate.
- Pacemakers are used to treat arrhythmias. Arrhythmias
are problems with the rate or rhythm of the heartbeat. During an arrhythmia, the heart can beat too fast,
too slow, or with an irregular rhythm.
- Pacemakers can relieve some arrhythmia symptoms, such
as fatigue (tiredness) and fainting. A pacemaker also can help a
person who has abnormal heart rhythms resume a more active lifestyle.
- Doctors also treat arrhythmias with implantable cardioverter defibrillators
- Doctors recommend pacemakers for a number of reasons.
The most common reasons are bradycardia and heart block.
Bradycardia is a slower than normal heartbeat. Heart block is a problem
that occurs with the heart's electrical system. The disorder occurs when
an electrical signal is slowed or disrupted as it moves through the heart.
- Before recommending a pacemaker, your doctor will
consider any arrhythmia symptoms you have, such as dizziness,
unexplained fainting,
or shortness
of breath. He or she also will consider whether you have a
history of heart
disease, what medicines you're currently taking, and the
results of heart tests.
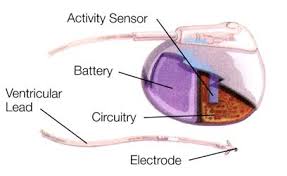
- A pacemaker consists of a battery, a computerized
generator, and wires with sensors called electrodes on one end. The
electrodes detect your heart's electrical activity and send data through
the wires to the computer in the generator.
- If your heart rhythm is abnormal, the computer will
direct the generator to send electrical pulses to your heart. The pulses
then travel through the wires to reach your heart.
- Newer pacemakers also can monitor your blood
temperature, breathing,
and other factors and adjust your heart rate to changes in your activity.
- Placing a pacemaker requires minor surgery. The surgery
usually is done in a hospital or special heart treatment laboratory. You'll
be given medicine just before the surgery that will help you relax and may
make you sleepy.
- The surgery takes just a few hours, but you'll stay in
the hospital overnight so your health care team can check your heartbeat
and make sure your pacemaker is working properly.
- Complications from pacemaker surgery are rare. Most
people can return to their normal activities within a few days.
- Your doctor may ask you to avoid vigorous exercise or
heavy lifting for about a month after your surgery. After you have fully
recovered from surgery, discuss with your doctor how much and what kinds
of physical activity are safe for you.
- Once you have a pacemaker, you have to avoid close or
prolonged contact with electrical devices or devices that have strong
magnetic fields. You also need to avoid certain medical procedures that
can disrupt your pacemaker.
- Let all of your doctors, dentists, and medical
technicians know that you have a pacemaker. Your doctor can give you a
card that states what kind of pacemaker you have. Carry this card in your
wallet. You may want to consider wearing a medical ID bracelet or necklace
that explains that you have a pacemaker.
- Your doctor will want to check your pacemaker regularly.
Some pacemaker functions can be checked remotely through a telephone call
or a computer connection to the Internet. Your doctor may ask you to come
to his or her office to check your pacemaker.
- Pacemaker batteries last between 5 and 15 years
(average 6 to 7 years), depending on how active your pacemaker is. The
wires of your pacemaker also may need to be replaced eventually. Your
doctor can tell you whether your pacemaker or its wires need to be
replaced.
Faulty electrical
signaling in the heart causes arrhythmias. Pacemakers use low-energy electrical
pulses to overcome this faulty electrical signaling. Pacemakers can:
- Speed up a slow heart rhythm.
- Help control an abnormal or fast heart rhythm.
- Make sure the ventricles contract normally if the atria
are quivering instead of beating with a normal rhythm (a condition called atrial
fibrillation).
- Coordinate electrical signaling between the upper and
lower chambers of the heart.
- Coordinate electrical signaling between the ventricles.
Pacemakers that do this are called cardiac resynchronization therapy (CRT)
devices. CRT devices are used to treat heart
failure.
- Prevent dangerous arrhythmias caused by a disorder
called long QT syndrome.
Pacemakers also can
monitor and record your heart's electrical activity and heart rhythm. Newer
pacemakers can monitor your blood temperature, breathing rate, and other
factors. They also can adjust your heart rate to changes in your activity.
Pacemakers can be
temporary or permanent. Temporary pacemakers are used to treat short-term heart
problems, such as a slow heartbeat that's caused by a heart attack,
heart surgery, or an overdose of medicine.
Temporary pacemakers
also are used during emergencies. They might be used until your doctor can
implant a permanent pacemaker or until a temporary condition goes away. If you
have a temporary pacemaker, you'll stay in a hospital as long as the device is in
place.
Permanent pacemakers
are used to control long-term heart rhythm problems. This article mainly
discusses permanent pacemakers, unless stated otherwise.
Doctors also treat
arrhythmias with another device called an implantable cardioverterdefibrillator (ICD).
An ICD is similar to a pacemaker. However, besides using low-energy electrical
pulses, an ICD also can use high-energy pulses to treat life-threatening
arrhythmias.
What is a pacemaker?
A pacemaker is a small device that's placed in the chest or abdomen
to help control abnormal heart rhythms. This device uses electrical pulses to
prompt the heart to beat at a normal rate.
Pacemakers are used to treat arrhythmias (ah-RITH-me-ahs).
Arrhythmias are problems with the rate or rhythm of the heartbeat. During an
arrhythmia, the heart can beat too fast, too slow, or with an irregular rhythm.
A heartbeat that's too fast is called tachycardia
(TAK-ih-KAR-de-ah). A heartbeat that's too slow is called bradycardia
(bray-de-KAR-de-ah).
During an arrhythmia, the heart may not be able to pump enough
blood to the body. This can cause symptoms such as fatigue (tiredness), shortness of breath, or
fainting. Severe arrhythmias can damage the body's vital organs and may even
cause loss of consciousnessor
death.
A pacemaker can relieve some arrhythmia symptoms, such asfatigue and fainting. A pacemaker also can
help a person who has abnormal heart rhythms resume a more active lifestyle.
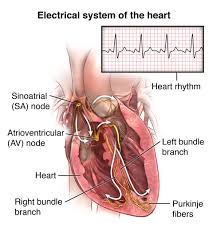
Understanding the
heart's electrical system
Your heart has its own internal electrical system that controls
the rate and rhythm of your heartbeat. With each heartbeat, an electrical
signal spreads from the top of your heart to the bottom. As the signal travels,
it causes the heart to contract and pump blood.
Each electrical signal normally begins in a group of cells
called the sinus node or sinoatrial (SA) node. As the signal spreads from the
top of the heart to the bottom, it coordinates the timing of heart cell
activity.
First, the heart's two upper chambers, the atria (AY-tree-uh),
contract. This contraction pumps blood into the heart's two lower chambers, the
ventricles (VEN-trih-kuls). The ventricles then contract and pump blood to the
rest of the body. The combined contraction of the atria and ventricles is a
heartbeat.
For more information about the heart's electrical system and
detailed animations, go to the Health Topics How the Heart
Works article.
What is a pacemaker?
A pacemaker is a small device that's placed in the chest or
abdomen to help control abnormal heart rhythms. This device uses electrical
pulses to prompt the heart to beat at a normal rate.
Pacemakers are used to treat arrhythmias (ah-RITH-me-ahs).
Arrhythmias are problems with the rate or rhythm of the heartbeat. During an
arrhythmia, the heart can beat too fast, too slow, or with an irregular rhythm.
A heartbeat that's too fast is called tachycardia
(TAK-ih-KAR-de-ah). A heartbeat that's too slow is called bradycardia (bray-de-KAR-de-ah).
During an arrhythmia, the heart may not be able to pump enough
blood to the body. This can cause symptoms such as fatigue (tiredness), shortness of breath, or
fainting. Severe arrhythmias can damage the body's vital organs and may even
cause loss of consciousnessor
death.
A pacemaker can relieve some arrhythmia symptoms, such asfatigue and fainting. A pacemaker also can
help a person who has abnormal heart rhythms resume a more active lifestyle.
Understanding
the heart's electrical system
Your heart has its own internal electrical system that controls
the rate and rhythm of your heartbeat. With each heartbeat, an electrical
signal spreads from the top of your heart to the bottom. As the signal travels,
it causes the heart to contract and pump blood.
Each electrical signal normally begins in a group of cells
called the sinus node or sinoatrial (SA) node. As the signal spreads from the
top of the heart to the bottom, it coordinates the timing of heart cell
activity.
First, the heart's two upper chambers, the atria (AY-tree-uh),
contract. This contraction pumps blood into the heart's two lower chambers, the
ventricles (VEN-trih-kuls). The ventricles then contract and pump blood to the
rest of the body. The combined contraction of the atria and ventricles is a
heartbeat.
For more information about the heart's electrical system and
detailed animations, go to the Health Topics How the Heart
Works article.
Who needs a pacemaker?
Doctors recommend
pacemakers for many reasons. The most common reasons are bradycardia and heart
block.
Bradycardia is a
heartbeat that is slower than normal. Heart block is a disorder that occurs if
an electrical signal is slowed or disrupted as it moves through the heart.
Heart block can happen
as a result of aging,
damage to the heart from a heart attack, or other conditions that disrupt the
heart's electrical activity. Some nerve and muscle disorders also can cause
heart block, including muscular dystrophy.
Your doctor also may
recommend a pacemaker if:
- Aging or heart disease damages
your sinus node's ability to set the correct pace for your heartbeat. Such
damage can cause slower than normal heartbeats or long pauses between
heartbeats. The damage also can cause your heart to switch between slow
and fast rhythms. This condition is called sick sinus syndrome.
- You've had a medical procedure to treat an arrhythmia
calledatrial fibrillation.
A pacemaker can help regulate your heartbeat after the procedure.
- You need to take certain heart medicines, such as beta
blockers. These medicines can slow your heartbeat too much.
- You faint or have other symptoms of a slow heartbeat.
For example, this may happen if the main artery in your neck that supplies
your brain with blood is sensitive to pressure. Just quickly turning your
neck can cause your heart to beat slower than normal. As a result, your
brain might not get enough blood flow, causing you to feel faint or
collapse.
- You have heart muscle problems
that cause electrical signals to travel too slowly through your heart
muscle. Your pacemaker may provide cardiac resynchronization therapy (CRT)
for this problem. CRT devices coordinate electrical signaling between the
heart's lower chambers.
- You have long QT syndrome, which puts you at risk for
dangerous arrhythmias.
Doctors also may
recommend pacemakers for people who have certain types of congenitalheart disease or for people who have had
heart transplants. Children, teens, and adults
can use pacemakers.
Before recommending a
pacemaker, your doctor will consider any arrhythmia symptoms you have, such as dizziness,
unexplained fainting, or shortness of breath. He or she also will consider
whether you have a history of heart disease, what medicines you're currently
taking, and the results of heart tests.
Diagnostic tests
Many tests are used to detect arrhythmias. You may have one or
more of the following tests.
EKG
(Electrocardiogram)
An EKG is
a simple, painless test that detects and records the heart's electrical
activity. The test shows how fast your heart is beating and its rhythm (steady
or irregular).
An EKG also records the strength and timing of electrical
signals as they pass through your heart. The test can help diagnose bradycardia
and heart block (the most common reasons for needing a pacemaker).
A standard EKG only records the heartbeat for a few seconds. It
won't detect arrhythmias that don't happen during the test.
To diagnose heart rhythm problems that come and go, your doctor
may have you wear a portable EKG monitor. The two most common types of portable
EKGs are Holter and event monitors. How does a pacemaker work?
·
Share Your Story
A pacemaker consists
of a battery, a computerized generator, and wires with sensors at their tips.
(The sensors are called electrodes.) The battery powers the generator, and both
are surrounded by a thin metal box. The wires connect the generator to the
heart.
A pacemaker helps
monitor and control your heartbeat. The electrodes detect your heart's
electrical activity and send data through the wires to the computer in the
generator.
If your heart rhythm
is abnormal, the computer will direct the generator to send electrical pulses
to your heart. The pulses travel through the wires to reach your heart.
Newer pacemakers can
monitor your blood temperature, breathing, and other factors. They also can
adjust your heart rate to changes in your activity.
The pacemaker's
computer also records your heart's electrical activity and heart rhythm. Your
doctor will use these recordings to adjust your pacemaker so it works better
for you.
Your doctor can
program the pacemaker's computer with an external device. He or she doesn't
have to use needles or have direct contact with the pacemaker.
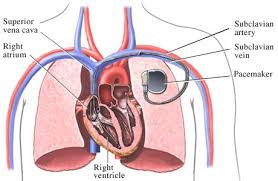
Pacemakers have one to
three wires that are each placed in different chambers of the heart.
- The wires in a single-chamber pacemaker usually carry
pulses from the generator to the right
ventricle (the lower right chamber of your heart).
- The wires in a dual-chamber pacemaker carry pulses from
the generator to theright
atrium (the upper right chamber of your heart) and the
right ventricle. The pulses help coordinate the timing of these two
chambers' contractions.
- The wires in a biventricular pacemaker carry pulses
from the generator to anatrium and
both ventricles. The pulses help coordinate electrical signaling between
the two ventricles. This type of pacemaker also is called a cardiac
resynchronization therapy (CRT) device.
How does a pacemaker work?
·
Share Your Story
A pacemaker consists
of a battery, a computerized generator, and wires with sensors at their tips.
(The sensors are called electrodes.) The battery powers the generator, and both
are surrounded by a thin metal box. The wires connect the generator to the
heart.
A pacemaker helps
monitor and control your heartbeat. The electrodes detect your heart's
electrical activity and send data through the wires to the computer in the
generator.
If your heart rhythm
is abnormal, the computer will direct the generator to send electrical pulses
to your heart. The pulses travel through the wires to reach your heart.
Newer pacemakers can
monitor your blood temperature, breathing, and other factors. They also can
adjust your heart rate to changes in your activity.
The pacemaker's
computer also records your heart's electrical activity and heart rhythm. Your
doctor will use these recordings to adjust your pacemaker so it works better
for you.
Your doctor can
program the pacemaker's computer with an external device. He or she doesn't
have to use needles or have direct contact with the pacemaker.
Pacemakers have one to
three wires that are each placed in different chambers of the heart.
- The wires in a single-chamber pacemaker usually carry
pulses from the generator to the right
ventricle (the lower right chamber of your heart).
- The wires in a dual-chamber pacemaker carry pulses from
the generator to theright
atrium (the upper right chamber of your heart) and the
right ventricle. The pulses help coordinate the timing of these two
chambers' contractions.
- The wires in a biventricular pacemaker carry pulses
from the generator to anatrium and
both ventricles. The pulses help coordinate electrical signaling between
the two ventricles. This type of pacemaker also is called a cardiac
resynchronization therapy (CRT) device.
Holter
and Event Monitors
A Holter monitor records the heart's electrical activity for a full
24- or 48-hour period. You wear one while you do your normal daily activities.
This allows the monitor to record your heart for a longer time than a standard
EKG.
An event monitor is similar to a Holter monitor. You wear an
event monitor while doing your normal activities. However, an event monitor
only records your heart's electrical activity at certain times while you're
wearing it.
For many event monitors, you push a button to start the monitor
when you feel symptoms. Other event monitors start automatically when they
sense abnormal heart rhythms.
You can wear an event monitor for weeks or until symptoms occur.
Echocardiography
Echocardiography (echo) uses sound waves to create a
moving picture of your heart. The test shows the size and shape of your heart
and how well your heart chambers and valves are working.
Echo also can show areas of poor blood flow to the heart, areas
of heart muscle that aren't contracting normally, and injury to the heart
muscle caused by poor blood flow.
Electrophysiology
Study
For this test, a thin, flexible wire is passed through a vein in
your groin (upper thigh) or arm to your heart. The wire records the heart's
electrical signals.
Your doctor uses the wire to electrically stimulate your heart.
This allows him or her to see how your heart's electrical system responds. This
test helps pinpoint where the heart's electrical system is damaged.
Stress
Test
Some heart problems are easier to diagnose when your heart is
working hard and beating fast.
During stress testing, you exercise to make your heart work hard and beat
fast while heart tests, such as an EKG or echo, are done. If you can't
exercise, you may be given medicine to raise your heart rate.
How Does a Pacemaker Work?
A pacemaker consists of a battery, a computerized generator, and wires with sensors at their tips. (The sensors are called electrodes.) The battery powers the generator, and both are surrounded by a thin metal box. The wires connect the generator to the heart.
A pacemaker helps monitor and control your heartbeat. The electrodes detect your heart's electrical activity and send data through the wires to the computer in the generator.
If your heart rhythm is abnormal, the computer will direct the generator to send electrical pulses to your heart. The pulses travel through the wires to reach your heart.
Newer pacemakers can monitor your blood temperature, breathing, and other factors. They also can adjust your heart rate to changes in your activity.
The pacemaker's computer also records your heart's electrical activity and heart rhythm. Your doctor will use these recordings to adjust your pacemaker so it works better for you.
Your doctor can program the pacemaker's computer with an external device. He or she doesn't have to use needles or have direct contact with the pacemaker.
Pacemakers have one to three wires that are each placed in different chambers of the heart.
- The wires in a single-chamber pacemaker usually carry pulses from the generator to the right ventricle (the lower right chamber of your heart).
- The wires in a dual-chamber pacemaker carry pulses from the generator to the right atrium (the upper right chamber of your heart) and the right ventricle. The pulses help coordinate the timing of these two chambers' contractions.
- The wires in a biventricular pacemaker carry pulses from the generator to an atrium and both ventricles. The pulses help coordinate electrical signaling between the two ventricles. This type of pacemaker also is called a cardiac resynchronization therapy (CRT) device.
What Is a Pacemaker?
A
pacemaker is a small device that's placed in the chest or abdomen to help
control abnormal heart rhythms. This device uses electrical pulses to prompt
the heart to beat at a normal rate.
Pacemakers are used to treat arrhythmias (ah-RITH-me-ahs). Arrhythmias are
problems with the rate or rhythm of the heartbeat. During an arrhythmia, the
heart can beat too fast, too slow, or with an irregular rhythm.
A heartbeat that's too fast is
called tachycardia (TAK-ih-KAR-de-ah). A heartbeat that's too slow is called
bradycardia (bray-de-KAR-de-ah).
During an arrhythmia, the heart
may not be able to pump enough blood to the body. This can cause symptoms such
as fatigue (tiredness), shortness of breath, or fainting. Severe arrhythmias
can damage the body's vital organs and may even cause loss of consciousness or death.
A pacemaker can relieve some
arrhythmia symptoms, such as fatigue and fainting. A pacemaker also can help a
person who has abnormal heart rhythms resume a more active lifestyle.
Understanding the Heart's Electrical
System
Your heart has its own internal
electrical system that controls the rate and rhythm of your heartbeat. With
each heartbeat, an electrical signal spreads from the top of your heart to the
bottom. As the signal travels, it causes the heart to contract and pump blood.
Each electrical signal normally
begins in a group of cells called the sinus node or sinoatrial (SA) node. As
the signal spreads from the top of the heart to the bottom, it coordinates the
timing of heart cell activity.
First, the heart's two upper
chambers, the atria (AY-tree-uh), contract. This contraction pumps blood into
the heart's two lower chambers, the ventricles (VEN-trih-kuls). The ventricles
then contract and pump blood to the rest of the body. The combined contraction
of the atria and ventricles is a heartbeat.
For more information about the
heart's electrical system and detailed animations, go to the Health Topics How the Heart Works article.
Overview
Faulty electrical signaling in
the heart causes arrhythmias. Pacemakers use low-energy electrical pulses to
overcome this faulty electrical signaling. Pacemakers can:
·
Speed up a slow heart rhythm.
·
Help control an abnormal or fast heart rhythm.
·
Make sure the ventricles contract normally if the atria are
quivering instead of beating with a normal rhythm (a condition called atrial fibrillation).
·
Coordinate electrical signaling between the upper and lower
chambers of the heart.
·
Coordinate electrical signaling between the ventricles. Pacemakers
that do this are called cardiac resynchronization therapy (CRT) devices. CRT
devices are used to treat heart failure.
·
Prevent dangerous arrhythmias caused by a disorder called long QT syndrome.
Pacemakers also can monitor and
record your heart's electrical activity and heart rhythm. Newer pacemakers can
monitor your blood temperature, breathing rate, and other factors. They also
can adjust your heart rate to changes in your activity.
Pacemakers can be temporary or
permanent. Temporary pacemakers are used to treat short-term heart problems,
such as a slow heartbeat that's caused by a heart attack, heart surgery, or
an overdose of medicine.
Temporary pacemakers also are
used during emergencies. They might be used until your doctor can implant a
permanent pacemaker or until a temporary condition goes away. If you have a
temporary pacemaker, you'll stay in a hospital as long as the device is in
place.
Permanent pacemakers are used
to control long-term heart rhythm problems. This article mainly discusses
permanent pacemakers, unless stated otherwise.
Doctors also treat arrhythmias
with another device called an implantable cardioverter
defibrillator (ICD).
An ICD is similar to a pacemaker. However, besides using low-energy electrical
pulses, an ICD also can use high-energy pulses to treat life-threatening
arrhythmias.
Who Needs a Pacemaker?
Doctors
recommend pacemakers for many reasons. The most common reasons are bradycardia
and heart block.
Bradycardia is a heartbeat that
is slower than normal. Heart block is a disorder that occurs if an electrical
signal is slowed or disrupted as it moves through the heart.
Heart block can happen as a
result of aging, damage to the heart from a heart attack, or
other conditions that disrupt the heart's electrical activity. Some nerve and
muscle disorders also can cause heart block, including muscular dystrophy.
Your doctor also may recommend
a pacemaker if:
·
Aging or heart disease damages your sinus node's ability to set
the correct pace for your heartbeat. Such damage can cause slower than normal
heartbeats or long pauses between heartbeats. The damage also can cause your
heart to switch between slow and fast rhythms. This condition is called sick
sinus syndrome.
·
You've had a medical procedure to treat an arrhythmia called atrial fibrillation.
A pacemaker can help regulate your heartbeat after the procedure.
·
You need to take certain heart medicines, such as beta blockers.
These medicines can slow your heartbeat too much.
·
You faint or have other symptoms of a slow heartbeat. For example,
this may happen if the main artery in your neck that supplies your brain with
blood is sensitive to pressure. Just quickly turning your neck can cause your
heart to beat slower than normal. As a result, your brain might not get enough
blood flow, causing you to feel faint or collapse.
·
You have heart muscle problems that cause electrical signals to
travel too slowly through your heart muscle. Your pacemaker may provide cardiac
resynchronization therapy (CRT) for this problem. CRT devices coordinate
electrical signaling between the heart's lower chambers.
·
You have long QT syndrome,
which puts you at risk for dangerous arrhythmias.
Doctors also may recommend
pacemakers for people who have certain types of congenital heart disease or for people who have had heart transplants.
Children, teens, and adults can use pacemakers.
Before recommending a
pacemaker, your doctor will consider any arrhythmia symptoms you have, such as
dizziness, unexplained fainting, or shortness of breath. He or she also will
consider whether you have a history of heart disease, what medicines you're
currently taking, and the results of heart tests.
Diagnostic Tests
Many tests are used to detect
arrhythmias. You may have one or more of the following tests.
EKG (Electrocardiogram)
An EKG is a simple, painless test that
detects and records the heart's electrical activity. The test shows how fast
your heart is beating and its rhythm (steady or irregular).
An EKG also records the
strength and timing of electrical signals as they pass through your heart. The
test can help diagnose bradycardia and heart block (the most common reasons for
needing a pacemaker).
A standard EKG only records the
heartbeat for a few seconds. It won't detect arrhythmias that don't happen
during the test.
To diagnose heart rhythm
problems that come and go, your doctor may have you wear a portable EKG
monitor. The two most common types of portable EKGs are Holter and event monitors.
Holter and Event Monitors
A Holter monitor records the
heart's electrical activity for a full 24- or 48-hour period. You wear one
while you do your normal daily activities. This allows the monitor to record
your heart for a longer time than a standard EKG.
An event monitor is similar to
a Holter monitor. You wear an event monitor while doing your normal activities.
However, an event monitor only records your heart's electrical activity at
certain times while you're wearing it.
For many event monitors, you
push a button to start the monitor when you feel symptoms. Other event monitors
start automatically when they sense abnormal heart rhythms.
You can wear an event monitor
for weeks or until symptoms occur.
Echocardiography
Echocardiography (echo) uses sound waves to create a
moving picture of your heart. The test shows the size and shape of your heart
and how well your heart chambers and valves are working.
Echo also can show areas of
poor blood flow to the heart, areas of heart muscle that aren't contracting
normally, and injury to the heart muscle caused by poor blood flow.
Electrophysiology Study
For this test, a thin, flexible
wire is passed through a vein in your groin (upper thigh) or arm to your heart.
The wire records the heart's electrical signals.
Your doctor uses the wire to
electrically stimulate your heart. This allows him or her to see how your
heart's electrical system responds. This test helps pinpoint where the heart's
electrical system is damaged.
Stress Test
Some heart problems are easier
to diagnose when your heart is working hard and beating fast.
During stress testing,
you exercise to make your heart work hard and beat fast while heart tests, such
as an EKG or echo, are done. If you can't exercise, you may be given medicine
to raise your heart rate.
Types of Pacemaker Programming
The two
main types of programming for pacemakers are demand pacing and rate-responsive
pacing.
A demand
pacemaker monitors your heart rhythm. It only sends electrical pulses to your
heart if your heart is beating too slow or if it misses a beat.
A
rate-responsive pacemaker will speed up or slow down your heart rate depending
on how active you are. To do this, the device monitors your sinus node rate,
breathing, blood temperature, and other factors to determine your activity
level.
Your
doctor will work with you to decide which type of pacemaker is best for you.
A
rate-responsive pacemaker will speed up or slow down your heart rate depending
on how active you are. To do this, the device monitors your sinus node rate,
breathing, blood temperature, and other factors to determine your activity
level.
What To Expect During Pacemaker Surgery
Placing
a pacemaker requires minor surgery. The surgery usually is done in a hospital
or special heart treatment laboratory.
Before the surgery, an
intravenous (IV) line will be inserted into one of your veins. You will receive
medicine through the IV line to help you relax. The medicine also might make
you sleepy.
Your doctor will numb the area
where he or she will put the pacemaker so you don't feel any pain. Your doctor
also may give you antibiotics to prevent infection.
First, your doctor will insert
a needle into a large vein, usually near the shoulder opposite your dominant
hand. Your doctor will then use the needle to thread the pacemaker wires into
the vein and to correctly place them in your heart.
An x-ray "movie" of
the wires as they pass through your vein and into your heart will help your
doctor place them. Once the wires are in place, your doctor will make a small
cut into the skin of your chest or abdomen.
He or she will slip the
pacemaker's small metal box through the cut, place it just under your skin, and
connect it to the wires that lead to your heart. The box contains the
pacemaker's battery and generator.
Once the pacemaker is in place,
your doctor will test it to make sure it works properly. He or she will then
sew up the cut. The entire surgery takes a few hours.
What To Expect After Pacemaker Surgery
Expect
to stay in the hospital overnight so your health care team can check your
heartbeat and make sure your pacemaker is working well. You'll likely have to
arrange for a ride to and from the hospital because your doctor may not want
you to drive yourself.
For a few days to weeks after
surgery, you may have pain, swelling, or tenderness in the area where your
pacemaker was placed. The pain usually is mild; over-the-counter medicines
often can relieve it. Talk to your doctor before taking any pain medicines.
Your doctor may ask you to
avoid vigorous activities and heavy lifting for about a month after pacemaker
surgery. Most people return to their normal activities within a few days of
having the surgery.
What Are the Risks of Pacemaker Surgery?
Pacemaker
surgery generally is safe. If problems do occur, they may include:
·
Swelling, bleeding, bruising, or infection in the area where the
pacemaker was placed
·
Blood vessel or nerve damage
·
A collapsed lung
·
A bad reaction to the medicine used during the procedure
Talk with your doctor about the
benefits and risks of pacemaker surgery.
How Will a Pacemaker Affect My Lifestyle?
Once
you have a pacemaker, you have to avoid close or prolonged contact with
electrical devices or devices that have strong magnetic fields. Devices that
can interfere with a pacemaker include:
·
Cell phones and MP3 players (for example, iPods)
·
Household appliances, such as microwave ovens
·
High-tension wires
·
Metal detectors
·
Industrial welders
·
Electrical generators
These
devices can disrupt the electrical signaling of your pacemaker and stop it from
working properly. You may not be able to tell whether your pacemaker has been
affected.
How
likely a device is to disrupt your pacemaker depends on how long you're exposed
to it and how close it is to your pacemaker.
To be
safe, some experts recommend not putting your cell phone or MP3 player in a
shirt pocket over your pacemaker (if the devices are turned on).
You may
want to hold your cell phone up to the ear that's opposite the site where your
pacemaker is implanted. If you strap your MP3 player to your arm while
listening to it, put it on the arm that's farther from your pacemaker.
You can
still use household appliances, but avoid close and prolonged exposure, as it
may interfere with your pacemaker.
You can
walk through security system metal detectors at your normal pace. Security
staff can check you with a metal detector wand as long as it isn't held for too
long over your pacemaker site. You should avoid sitting or standing close to a
security system metal detector. Notify security staff if you have a pacemaker.
Also,
stay at least 2 feet away from industrial welders and electrical generators.
Some
medical procedures can disrupt your pacemaker. These procedures include:
·
Magnetic resonance imaging, or MRI
·
Shock-wave lithotripsy to get rid of kidney stones
·
Electrocauterization to stop bleeding during surgery
Let all
of your doctors, dentists, and medical technicians know that you have a
pacemaker. Your doctor can give you a card that states what kind of pacemaker
you have. Carry this card in your wallet. You may want to wear a medical ID
bracelet or necklace that states that you have a pacemaker.
Physical
Activity
In most
cases, having a pacemaker won't limit you from doing sports and exercise,
including strenuous activities.
You may
need to avoid full-contact sports, such as football. Such contact could damage
your pacemaker or shake loose the wires in your heart. Ask your doctor how much
and what kinds of physical activity are safe for you.
Ongoing Care
Your
doctor will want to check your pacemaker regularly (about every 3 months). Over
time, a pacemaker can stop working properly because:
·
Its wires get dislodged or broken
·
Its battery gets weak or fails
·
Your heart disease progresses
·
Other devices have disrupted its electrical signaling
To check
your pacemaker, your doctor may ask you to come in for an office visit several
times a year. Some pacemaker functions can be checked remotely using a phone or
the Internet.
Your
doctor also may ask you to have an EKG (electrocardiogram) to check for changes
in your heart's electrical activity.
Battery
Replacement
Pacemaker
batteries last between 5 and 15 years (average 6 to 7 years), depending on how
active the pacemaker is. Your doctor will replace the generator along with the
battery before the battery starts to run down.
Replacing
the generator and battery is less-involved surgery than the original surgery to
implant the pacemaker. Your pacemaker wires also may need to be replaced
eventually.