Medi Services

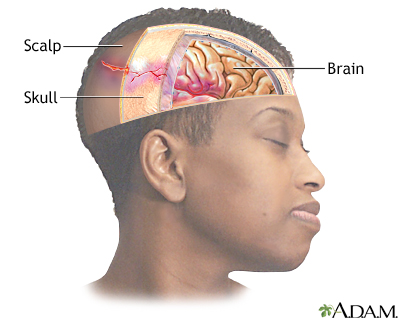
A head injury is any sort of injury to your brain, skull, or scalp. This can range from a mild bump or bruise to a traumatic brain injury. Common head injuries include concussions, skull fractures, and scalp wounds. The consequences and treatments vary greatly, depending on what caused your head injury and how severe it is.
Head injuries may be either closed or open. A closed head injury is any injury that doesn’t break your skull. An open, or penetrating, head injury is one in which something breaks your skull and enters your brain.
It can be hard to assess how serious a head injury is just by looking. Some minor head injuries bleed a lot, while some major injuries don’t bleed at all. It’s important to treat all head injuries seriously and get them assessed by a doctor.
What Causes a Head Injury?In general, head injuries can be divided into two categories based on what causes them. They can either be head injuries due to blows to the head or head injuries due to shaking.
Head injuries caused by shaking are most common in infants and small children, but they can occur any time you experience violent shaking.
Head injuries caused by a blow to the head are usually associated with:
In most cases, your skull will protect your brain from serious harm.
What Are the Major Types of Head Injuries?
A hematoma is a collection, or clotting, of blood outside the blood vessels. It can be very serious if a hematoma occurs in the brain. The clotting can cause pressure to build inside your skull, which can cause you to lose consciousness.
A hemorrhage is uncontrolled bleeding. There can be bleeding in the space around your brain, which is a subarachnoid hemorrhage, or bleeding within your brain tissue, which is an intracerebral hemorrhage.
Subarachnoid bleeds often cause headaches and vomiting. The severity of intracerebral hemorrhages depends on how much bleeding there is, but over time any amount of blood can cause pressure to build.
A concussion is a brain injury that occurs when your brain bounces against the hard walls of your skull. Generally speaking, the loss of function associated with concussions is temporary. However, repeated concussions can eventually lead to permanent damage.
Any brain injury can lead to edema, or swelling. Many injuries cause swelling of the surrounding tissues, but it’s more serious when it occurs in your brain. Your skull can’t stretch to accommodate the swelling, which leads to a buildup of pressure in your brain. This can cause your brain to press against your skull.
Unlike most bones in your body, your skull doesn’t have bone marrow. This makes the skull very strong and difficult to break. A broken skull is unable to absorb the impact, making it more likely that there will also be damage to your brain.
A diffuse axonal injury, or sheer injury, is an injury to the brain that doesn’t cause bleeding but does damage your brain cells. Though it isn’t as outwardly visible as other forms of brain injury, diffuse axonal injury is one of the most dangerous types of head injuries and can lead to permanent brain damage and even death.
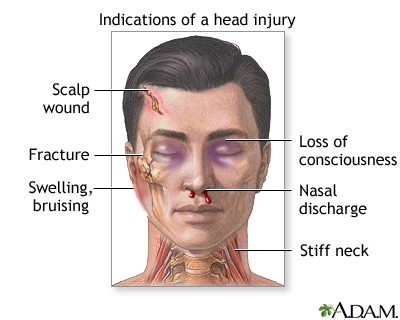
What Are the Symptoms of a Head Injury?Your head has more blood vessels than any other part of your body, so bleeding on the surface of your brain or within your brain is a serious concern in head injuries. However, not all head injuries cause bleeding. It’s important to be aware of other symptoms to watch out for. Many symptoms of serious brain injury won’t appear right away. You should always continue to monitor your symptoms for several days after you injure your head.
Common symptoms of a minor head injury include:
The symptoms of a severe head injury include many of the symptoms of minor head injuries. They can also include:
When Does a Head Injury Require Medical Attention?
Head injuries shouldn’t be taken lightly. See your doctor right away if you think you have the symptoms of a serious head injury.
In particular, you should always call 911 or go to an emergency room if you experience loss of consciousness, confusion, or disorientation. Even if you don’t go to the ER immediately after the accident, you should seek help if you still have symptoms after a day or two.
In the case of a potentially serious head injury, you should always call 911. Motion can sometimes make a head injury worse, and emergency medical personnel are trained to move patients carefully without causing more damage.
Your doctor will need to know the circumstances of your injury. Often, if you have suffered a head injury, you won’t remember the details of the accident. If it’s possible, you should bring someone with you who witnessed the accident. It will be important for your doctor to determine if you lost consciousness and for how long if you did.
Your doctor will also examine you to look for signs of trauma, including bruising and swelling. You’re also likely to get a neurological examination, in which your doctor will evaluate your nerve function by assessing your muscle control and strength, eye movement, and sensation, among other things.
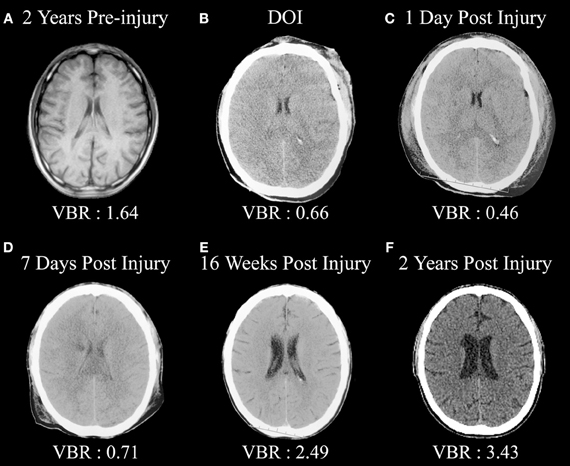
Imaging tests are commonly used to diagnose head injuries. A CT scan will help your doctor look for fractures, evidence of bleeding and clotting, brain swelling, and any other structural damage. CT scans are fast and accurate, so they’re typically the first type of imaging you will receive. You may also receive an MRI scan, which can offer a more detailed view of the brain. An MRI scan will usually only be ordered once you’re in stable condition.
Head injury can be either closed or open (penetrating).
Head injuries include:
Head injuries may cause bleeding:
Head injury is a common reason for an emergency room visit. A large number of people who suffer head injuries are children. TBI (traumatic brain injury) accounts for over 1 in 6 injury-related hospital admissions each year.
Common causes of head injury include:
Most of these injuries are minor because the skull protects the brain. Some injuries are severe enough to require a stay in the hospital.
Head injuries may cause bleeding in the brain tissue and the layers that surround the brain (subarachnoid hemorrhage, subdural hematomata extradural hematoma).
Symptoms of a head injury can occur right away. Or symptoms develop slowly over several hours or days. Even if the skull is not fractured, the brain can hit the inside of the skull and be bruised. The head may look fine, but problems could result from bleeding or swelling inside the skull.
The spinal cord is also likely to be injured in any serious trauma.
Some head injuries cause changes in brain function. This is called a traumatic brain injury. Concussion is a mild traumatic brain injury. Symptoms of a concussion can range from mild to severe.
Learning to recognize a serious head injury and give basic first aid can save someone's life. For a moderate to severe head injury, CALL 911 RIGHT AWAY.
Get medical help right away if the person:
Then take the following steps:
A serious head injury that involves bleeding or brain damage must be treated in a hospital.
For a mild head injury, no treatment may be needed. However, watch for symptoms of a head injury, which can which can show up later.
Your health care provider will explain what to expect, how to manage any headaches, how to treat your other symptoms, when to return to sports, school, work, and other activities, and signs or symptoms to worry about.
Both adults and children must follow the health care provider's instructions about when it will be possible to return to sports.
Call 911 right away if:
Head injuries include both injuries to the brain and those to other parts of the head, such as the scalp and skull.Head injuries can be closed or open. A closed (non-missile) head injury is where the dura mater remains intact. The skull can be fractured, but not necessarily. A penetrating head injury occurs when an object pierces the skull and breaches the dura mater. Brain injuries may be diffuse, occurring over a wide area, or focal, located in a small, specific area.A head injury may cause skull fracture, which may or may not be associated with injury to the brain. Some patients may have linear or depressed skull fractures.If intracranial hemorrhage occurs, a hematoma within the skull can put pressure on the brain. Types of intracranial hemorrage include subdural, subarachnoid, extradural, andintraparenchymal hematoma. Craniotomy surgeries are used in these cases to lessen the pressure by draining off blood.
Brain injury can be at the site of impact, but can also be at the opposite side of the skull due to a contrecoup effect (the impact to the head can cause the brain to move within the skull, causing the brain to impact the interior of the skull opposite the head-impact).If the impact causes the head to move, the injury may be worsened, because the brain may ricochet inside the skull causing additional impacts, or the brain may stay relatively still (due to inertia) but be hit by the moving skull (both are contrecoup injuries).
Specific problems after head injury can include[citation needed]:
A slightly greater injury is associated with both anterograde and retrograde amnesia (inability to remember events before or after the injury). The amount of time that the amnesia is present correlates with the severity of the injury. In all cases the patients develop postconcussion syndrome, which includes memory problems, dizziness, tiredness, sickness and depression.Cerebral concussion is the most common head injury seen in children.
| Hematoma type | Epidural | Subdural |
|---|---|---|
| Location | Between the skull and the outer endosteal layer of the dura mater | Between the dura and the arachnoid |
| Involved vessel | Temperoparietal locus (most likely) - Middle meningeal artery Frontal locus - anterior ethmoidal artery Occipital locus - transverse or sigmoid sinuses Vertex locus - superior sagittal sinus | Bridging veins |
| Symptoms(depend on severity) | Lucid interval followed by unconsciousness | Gradually increasing headache and confusion |
| CT appearance | Biconvex lens | Crescent-shaped |
Extra-axial hemorrhage, bleeding that occurs within the skull but outside of the brain tissue, falls into three subtypes:
Presentation varies according to the injury. Some patients with head trauma stabilize and other patients deteriorate. A patient may present with or without neurological deficit.Patients with concussion may have a history of seconds to minutes unconsciousness, then normal arousal. Disturbance of vision and equilibrium may also occur.Common symptoms of head injury include coma, confusion, drowsiness, personality change, seizures, nausea and vomiting, headache and a lucid interval, during which a patient appears conscious only to deteriorate later.[8]
Symptoms of skull fracture can include:
Because brain injuries can be life-threatening, even people with apparently slight injuries, with no noticeable signs or complaints, require close observation; They have a chance for severe symptoms later on. The caretakers of those patients with mild trauma who are released from the hospital are frequently advised to rouse the patient several times during the next 12 to 24 hours to assess for worsening symptoms.
The Glasgow Coma Scale (GCS) is a tool for measuring degree of unconsciousness and is thus a useful tool for determining severity of injury. The Pediatric Glasgow Coma Scale is used in young children. The widely used PECARN Pediatric Head Injury/Trauma Algorithm helps physicians weigh risk-benefit of imaging in a clinical setting given multiple factors about the patient - including mechanism/location of injury, age of patient, and GCS score.[9]
Common causes of head injury are motor vehicle traffic collisions, home and occupational accidents, falls, and assaults. Wilson's disease has also been indicative of head injury.[10]According to the United States CDC, 32% of traumatic brain injuries (another, more specific, term for head injuries) are caused by falls, 10% by assaults, 16.5% by being struck or against something, 17% by motor vehicle accidents, 21% by other/unknown ways. In addition, the highest rate of injury is among children ages 0–14 and adults age 65 and older.[11]
Clinicians will often consult clinical decision support rules such as the Canadian CT Head Rule or the New Orleans/Charity Head injury/Trauma Rule to decide if the patient needs further imaging studies or observation only. Rules like these are usually studied in depth by multiple research groups with large patient cohorts to ensure accuracy given the risk of adverse events in this area.[14]
In children with uncomplicated minor head injuries the risk of intra cranial bleeding over the next year is rare at 2 cases per 1 million.[15]In some cases transient neurological disturbances may occur, lasting minutes to hours. Malignant post traumatic cerebral swelling can develop unexpectedly in stable patients after an injury, as can post traumatic seizures. Recovery in children with neurologic deficits will vary. Children with neurologic deficits who improve daily are more likely to recover, while those who are vegetative for months are less likely to improve. Most patients without deficits have full recovery. However, persons who sustain head trauma resulting in unconsciousness for an hour or more have twice the risk of developing Alzheimer's disease later in life.[16]
Head injury may be associated with a neck injury. Bruises on the back or neck, neck pain, or pain radiating to the arms are signs of cervical spine injury and merit spinal immobilization via application of acervical collar and possibly a long board.If the neurological exam is normal this is reassuring. Reassessment is needed if there is a worsening headache, seizure, one sided weakness, or has persistent vomiting.
To combat overuse of Head CT Scans yielding negative intracranial hemorrhage, which unnecessarily expose patients to radiation and increase time in the hospital and cost of the visit, multiple clinical decision support rules have been developed to help clinicians weigh the option to scan a patient with a head injury. Among these are the Canadian Head CT rule, the PECARN Head Injury/Trauma Algorithm, and the New Orleans/Charity Head Injury/Trauma Rule all help clinicians make these decisions using easily obtained information and noninvasive practices.