Medi Services
A diabetic foot is a foot that exhibits any pathology that results directly from diabetes mellitus or any long-term (or "chronic") complication of diabetes mellitus.[1] Presence of several characteristic diabetic foot pathologies such as infection, diabetic foot ulcer and neuropathic osteoarthropathy is called diabetic foot syndrome.
Due to the peripheral nerve dysfunction associated with diabetes (diabetic neuropathy), patients have a reduced ability to feel pain. This means that minor injuries may remain undiscovered for a long while. People with diabetes are also at risk of developing a diabetic foot ulcer. Research estimates that the lifetime incidence of foot ulcers within the diabetic community is around 15% and may become as high as 25%.[2]
In diabetes, peripheral nerve dysfunction can be combined with peripheral artery disease (PAD) causing poor blood circulation to the extremities (diabetic angiopathy). Around half of patients with a diabetic foot ulcer have co-existing PAD.[3]
Where wounds take a long time to heal, infection may set in and lower limb amputation may be necessary. Foot infection is the most common cause of non-traumatic amputation in people with diabetes.[4]
n diabetes, there are two main types of diabetic foot, each of which has a characteristic form of ulceration: neuropathic and neuroischaemic foot. Neuropathic foot develops ulceration at the sites of high mechanical pressure on the plantar surface. Neuropathic ulcers also result from thermal or chemical injuries that are unperceived by the patients because of loss of pain sensation. Neuropathy is associated with an 8- to 18-fold higher risk of ulceration and a 2- to 15- fold higher risk of amputation. The mechanisms through which neuropathy acts as a pathogenetic event for ulceration, and thus amputation, are complex and different. Above all, the reduction of protective sensitivity (including sensitivity to pain and heat) leads to a reduction in the perception of pain stimuli. Moreover, the motor component of neuropathy involves a progressive weakening of the intrinsic muscle component made up of interosseous and lumbrical muscles. It reveals itself as a deformation in toe flexion and the formation of overloaded plantar areas, identifiable from under the metatarsal heads and the tips of the toes
The autonomous component of neuropathy causes anhydrosis and dry, flaky skin, as well as an increase in arterio-venous shunting, leading to altered skin and bone perfusion. It has been widely demonstrated that a biomechanical foot alteration, which includes an increase in plantar pressures, bone abnormalities, mobility limitations, and equinus, is all linked to a significant increase in the risk of ulceration. The clinical characteristics of the neuropathic lesion are the development of an overloaded area surrounded by a callous formation before the development of the lesion, without painful symptoms. The risk of the lesion worsening in terms both of progressive deep tissue destruction and of infection is linked to the co-existence of an ischaemic component. Therefore, PVD must be excluded in the initial assessment of an ulcerated lesion, verifying that its clinical characteristics are proper to those of a neuropathic lesion.
The literature clearly highlights how offloading is essential in cases of plantar neuropathic lesion. Simple offloading techniques are multifaceted and include casts and boots, sandals, half shoes, or felted foam dressings. The use of a non-removable cast has recently been shown to be faster treatment for plantar neuropathic ulcers than a half-shoe.
The first step in treating an uncomplicated ulcerated neuropathic lesion is local debridement, dressing, and offloading. However, clinical conditions exist in which surgery becomes the treatment of choice. Indications for the surgical treatment of plantar neuropathic ulcers are essentially:
The neuroischaemic foot has both neuropathy and ischaemia. It develops ulcers on the margins of the foot and toes, often at sites of pressure from poorly fitted shoes.
This pressure is unperceived because of a coexisting neuropathy. The main characteristic of PVD in diabetics is the morphological and clinical presentation.15 Painful symptoms are often reduced or absent due to the co-existence of neuropathic sensitivity, and medial arterial calcinosis is common. These features make PVD in diabetics more difficult to diagnose and therapy more problematic than in non-diabetics. They also mean that PVD plays a fundamental role in the prognosis of major amputation. Nevertheless, since the 1990s, revascularization procedures have been demonstrated to be feasible options, contrary to the initial thinking. Procedures ranging from distal revascularization to angioplasty and bypass interventions have all shown that they can change the original prognosis for amputation. Certainly, endoluminal or surgical revascularization is the only treatment capable of reducing the number of major amputations significantly. Revascularization can restore direct arterial flow where it has been interrupted or significantly reduced. This is an indispensable condition for healing a wound in an ischemic foot without resorting to amputation.If you have diabetes, your blood glucose, or blood sugar, levels are too high. Over time, this can damage your nerves or blood vessels. Nerve damage from diabetes can cause you to lose feeling in your feet. You may not feel a cut, a blister or a sore. Foot injuries such as these can cause ulcers and infections. Serious cases may even lead to amputation. Damage to the blood vessels can also mean that your feet do not get enough blood and oxygen. It is harder for your foot to heal, if you do get a sore or infection.
You can help avoid foot problems. First, control your blood sugar levels. Good foot hygiene is also crucial:
Inspect your feet every day, and seek care early if you do get a foot injury. Make sure your health care provider checks your feet at least once a year - more often if you have foot problems. Your health care provider should also give you a list and explain the do's and don'ts of foot care.
Most people can prevent any serious foot problem by following some simple steps. So let's begin taking care of your feet today.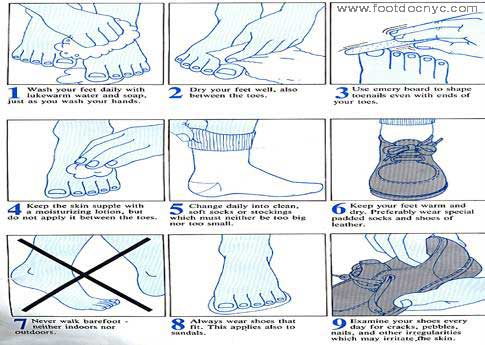
People with diabetes can develop many different foot problems. Even ordinary problems can get worse and lead to serious complications.
Foot problems most often happen when there is nerve damage, also called neuropathy. This can cause tingling, pain (burning or stinging), or weakness in the foot. It can also cause loss of feeling in the foot, so you can injure it and not know it. Poor blood flow or changes in the shape of your feet or toes may also cause problems.
Although it can hurt, diabetic nerve damage can also lessen your ability to feel pain, heat, and cold. Loss of feeling often means you may not feel a foot injury. You could have a tack or stone in your shoe and walk on it all day without knowing. You could get a blister and not feel it. You might not notice a foot injury until the skin breaks down and becomes infected.
Nerve damage can also lead to changes in the shape of your feet and toes. Ask your health care provider about special therapeutic shoes, rather than forcing deformed feet and toes into regular shoes.
Diabetes can cause changes in the skin of your foot. At times your foot may become very dry. The skin may peel and crack. The problem is that the nerves that control the oil and moisture in your foot no longer work.
After bathing, dry your feet and seal in the remaining moisture with a thin coat of plain petroleum jelly, an unscented hand cream, or other such products.
Do not put oils or creams between your toes. The extra moisture can lead to infection. Also, don't soak your feet — that can dry your skin.
Calluses occur more often and build up faster on the feet of people with diabetes. This is because there are high-pressure areas under the foot. Too much callus may mean that you will need therapeutic shoes and inserts.
Calluses, if not trimmed, get very thick, break down, and turn into ulcers (open sores). Never try to cut calluses or corns yourself - this can lead to ulcers and infection. Let your health care provider cut your calluses. Also, do not try to remove calluses and corns with chemical agents. These products can burn your skin.
Using a pumice stone every day will help keep calluses under control. It is best to use the pumice stone on wet skin. Put on lotion right after you use the pumice stone.
Ulcers occur most often on the ball of the foot or on the bottom of the big toe. Ulcers on the sides of the foot are usually due to poorly fitting shoes. Remember, even though some ulcers do not hurt, every ulcer should be seen by your health care provider right away. Neglecting ulcers can result in infections, which in turn can lead to loss of a limb.
What your health care provider will do varies with your ulcer. Your health care provider may take x-rays of your foot to make sure the bone is not infected. The health care provider may clean out any dead and infected tissue. You may need to go into the hospital for this. Also, the health care provider may culture the wound to find out what type of infection you have, and which antibiotic will work best.
Keeping off your feet is very important. Walking on an ulcer can make it get larger and force the infection deeper into your foot. Your health care provider may put a special shoe, brace, or cast on your foot to protect it.
If your ulcer is not healing and your circulation is poor, your health care provider may need to refer you to a vascular surgeon. Good diabetes control is important. High blood glucose levels make it hard to fight infection.
After the foot ulcer heals, treat your foot carefully. Scar tissue under the healed wound will break down easily. You may need to wear special shoes after the ulcer is healed to protect this area and to prevent the ulcer from returning.
Poor circulation (blood flow) can make your foot less able to fight infection and to heal. Diabetes causes blood vessels of the foot and leg to narrow and harden. You can control some of the things that cause poor blood flow. Don't smoke; smoking makes arteries harden faster. Also, follow your health care provider's advice for keeping your blood pressure and cholesterol under control.
If your feet are cold, you may be tempted to warm them. Unfortunately, if your feet cannot feel heat, it is easy for you to burn them with hot water, hot water bottles, or heating pads. The best way to help cold feet is to wear warm socks.
Some people feel pain in their calves when walking fast, up a hill, or on a hard surface. This condition is called intermittent claudication. Stopping to rest for a few moments should end the pain. If you have these symptoms, you must stop smoking. Work with your health care provider to get started on a walking program. Some people can be helped with medication to improve circulation.
Exercise is good for poor circulation. It stimulates blood flow in the legs and feet. Walk in sturdy, good-fitting, comfortable shoes, but don't walk when you have open sores.
People with diabetes are far more likely to have a foot or leg amputated than other people. The problem? Many people with diabetes have peripheral arterial disease (PAD), which reduces blood flow to the feet. Also, many people with diabetes have nerve disease, which reduces sensation. Together, these problems make it easy to get ulcers and infections that may lead to amputation. Most amputations are preventable withregular care and proper footwear.
For these reasons, take good care of your feet and see your health care provider right away about foot problems. Ask about prescription shoes that are covered by Medicare and other insurance. Always follow your health care provider's advice when caring for ulcers or other foot problems.
One of the biggest threats to your feet is smoking. Smoking affects small blood vessels. It can cause decreased blood flow to the feet and make wounds heal slowly. A lot of people with diabetes who need amputations are smokers.
Diabetes can harm your feet in a number of ways. It reduces blood flow to certain areas of the body, especially the legs and feet, which makes it harder for your body to heal injuries. Diabetes nerve damage may cause you to no longer feel pain in your feet, and you may not realize you have a wound or injury that needs treatment.
Diabetic nerve damage appears to be more common in people with the following conditions:
If you experience any of these symptoms, contact your health care provider or a podiatrist (foot doctor) right away.