Medi Services

Peptic ulcer disease refers to painful sores or ulcers in the lining of thestomach or first part of the small intestine, called the duodenum.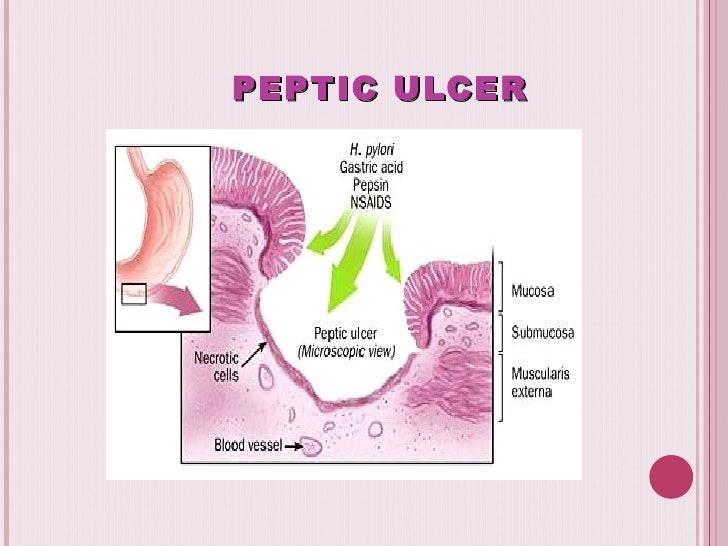
No single cause has been found for ulcers. However, it is now clear that an ulcer is the end result of an imbalance between digestive fluids in the stomach and duodenum. Most ulcers are caused by an infection with a type of bacteria called Helicobacter pylori (H. pylori).
Factors that can increase your risk for ulcers include:
An ulcer may or may not have symptoms. When symptoms occur, they may include:
In severe cases, symptoms can include:
Though ulcers often heal on their own, you shouldn't ignore their warning signs. If not properly treated, ulcers can lead to serious health problems, including:
Taking NSAIDs can lead to an ulcer without any warning. The risk is especially concerning for the elderly and for those with a prior history of having peptic ulcer disease.
You may be more likely to develop ulcers if you:
Your doctor may suspect you have an ulcer just by talking with you about your symptoms. However, to confirm the diagnosis one of several tests should be taken. First, your doctor may ask you to take an acid-blocking medication, such as those used to treat heartburn, for a short period of time to see if symptoms improve.
If needed, your doctor may recommend a procedure called anupper endoscopy. It involves inserting a small, lighted tube (endoscope) through the throat and into the stomach to look for abnormalities. This procedure is usually given if you are having severe or recurring symptoms of ulcers.
Doctors sometimes treat for ulcers without confirming the diagnosis using endoscopy.
Peptic ulcer disease (PUD), also known as a peptic ulcer or stomach ulcer, is a break in the lining of the stomach, first part of the small intestine, or occasionally the lower esophagus.[1][2] An ulcer in the stomach is known as a gastric ulcer while that in the first part of the intestines is known as a duodenal ulcer. The most common symptoms are waking at night with upper abdominal pain or upper abdominal pain that improves with eating. The pain is often described as a burning or dull ache. Other symptoms include belching, vomiting, weight loss, or poor appetite. About a third of older people have no symptoms.[1] Complications may include bleeding, perforation, and blockage of the stomach. Bleeding occurs in as many as 15% of people.[3]
Common causes include the bacteria Helicobacter pylori and non-steroidal anti-inflammatory drugs (NSAIDs).[1] Other less common causes include tobacco smoking, stress due to serious illness, Behcet disease, Zollinger-Ellison syndrome, Crohn disease and liver cirrhosis, among others.[1][4] Older people are more sensitive to the ulcer causing effects of NSAIDs. The diagnosis is typically suspected due to the presenting symptoms with confirmation by either endoscopyor barium swallow. H. pylori can be diagnosed by testing the blood for antibodies, a urea breath test, testing the stool for signs of the bacteria, or a biopsy of the stomach. Other conditions that produce similar symptoms include stomach cancer, coronary heart disease, and inflammation of the stomach lining orgallbladder.[1]
Diet does not play an important role in either causing or preventing ulcers.[5] Treatment includes stopping smoking, stopping NSAIDs, stopping alcohol, and medications to decrease stomach acid. The medication used to decrease acid is usually either a proton pump inhibitor (PPI) or an H2 blocker with four weeks of treatment initially recommended.[1] Ulcers due to H. pylori are treated with a combination of medications such as amoxicillin, clarithromycin, and a PPI.Antibiotic resistance is increasing and thus treatment may not always be effective.[6] Bleeding ulcers may be treated by endoscopy, with open surgery typically only used in cases in which it is not successful.[3]
A major causative factor (60% of gastric and up to 50-75%[16] of duodenal ulcers) is chronic inflammation due to Helicobacter pylori that colonizes the antral mucosa.[17] The immune system is unable to clear the infection, despite the appearance of antibodies. Thus, the bacterium can cause a chronic active gastritis (type B gastritis). Gastrin stimulates the production of gastric acid by parietal cells. In H. pylori colonization responses to increased gastrin, the increase in acid can contribute to the erosion of the mucosa and therefore ulcer formation.
Another major cause is the use of NSAIDs. The gastric mucosa protects itself from gastric acid with a layer of mucus, the secretion of which is stimulated by certain prostaglandins. NSAIDs block the function of cyclooxygenase 1 (cox-1), which is essential for the production of these prostaglandins. COX-2 selective anti-inflammatories (such as celecoxib or the since withdrawn rofecoxib) preferentially inhibit cox-2, which is less essential in the gastric mucosa, and roughly halve the risk of NSAID-related gastric ulceration.
Stress due to serious health problems such as those requiring treatment in an intensive care unit is well described as a cause of peptic ulcers, which are termed stress ulcers.[4]
While chronic life stress was once believed to be the main cause of ulcers, this is no longer the case.[18] It is, however, still occasionally believed to play a role.[18] This may be by increasing the risk in those with other causes such as H. pylori or NSAID use.[19]
Dietary factors such as spice consumption, were hypothesized to cause ulcers until late in the 20th century, but have been shown to be of relatively minor importance.[20] Caffeine and coffee, also commonly thought to cause or exacerbate ulcers, appear to have little effect.[21][22] Similarly, while studies have found that alcohol consumption increases risk when associated with H. pylori infection, it does not seem to independently increase risk. Even when coupled with H. pylori infection, the increase is modest in comparison to the primary risk factor.[23][24][nb 1]
Although some studies have found correlations between smoking and ulcer formation,[25] others have been more specific in exploring the risks involved and have found that smoking by itself may not be much of a risk factor unless associated with H. pylori infection.[23][26][27][nb 2]
Gastrinomas (Zollinger–Ellison syndrome), rare gastrin-secreting tumors, also cause multiple and difficult-to-heal ulcers.
The diagnosis is mainly established based on the characteristic symptoms. Stomach pain is usually the first signal of a peptic ulcer. In some cases, doctors may treat ulcers without diagnosing them with specific tests and observe whether the symptoms resolve, thus indicating that their primary diagnosis was accurate.
More specifically, peptic ulcers erode the muscularis mucosae, at least to the level of the submucosa (contrast with erosions, which do not involve the muscularis mucosae).[28]
Confirmation of the diagnosis is made with the help of tests such as endoscopies or barium contrast x-rays. The tests are typically ordered if the symptoms do not resolve after a few weeks of treatment, or when they first appear in a person who is over age 45 or who has other symptoms such as weight loss, becausestomach cancer can cause similar symptoms. Also, when severe ulcers resist treatment, particularly if a person has several ulcers or the ulcers are in unusual places, a doctor may suspect an underlying condition that causes the stomach to overproduce acid.[12]
An esophagogastroduodenoscopy (EGD), a form of endoscopy, also known as a gastroscopy, is carried out on patients in whom a peptic ulcer is suspected. By direct visual identification, the location and severity of an ulcer can be described. Moreover, if no ulcer is present, EGD can often provide an alternative diagnosis.
One of the reasons that blood tests are not reliable for accurate peptic ulcer diagnosis on their own is their inability to differentiate between past exposure to the bacteria and current infection. Additionally, a false negative result is possible with a blood test if the patient has recently been taking certain drugs, such asantibiotics or proton-pump inhibitors.[29]
The diagnosis of Helicobacter pylori can be made by:
The breath test uses radioactive carbon to detect H. pylori.[30] To perform this exam the patient will be asked to drink a tasteless liquid which contains the carbon as part of the substance that the bacteria breaks down. After an hour, the patient will be asked to blow into a bag that is sealed. If the patient is infected with H. pylori, the breath sample will contain radioactive carbon dioxide. This test provides the advantage of being able to monitor the response to treatment used to kill the bacteria.
The possibility of other causes of ulcers, notably malignancy (gastric cancer) needs to be kept in mind. This is especially true in ulcers of the greater (large) curvature of the stomach; most are also a consequence of chronic H. pylori infection.
If a peptic ulcer perforates, air will leak from the inside of the gastrointestinal tract (which always contains some air) to the peritoneal cavity (which normally never contains air). This leads to "free gas" within the peritoneal cavity. If the patient stands erect, as when having a chest X-ray, the gas will float to a position underneath the diaphragm. Therefore, gas in the peritoneal cavity, shown on an erect chest X-ray or supine lateral abdominal X-ray, is an omen of perforated peptic ulcer disease.
Gastric ulcers are most often localized on the lesser curvature of the stomach. The ulcer is a round to oval parietal defect ("hole"), 2 to 4 cm diameter, with a smooth base and perpendicular borders. These borders are not elevated or irregular in the acute form of peptic ulcer, regular but with elevated borders and inflammatory surrounding in the chronic form. In the ulcerative form of gastric cancer the borders are irregular. Surrounding mucosa may present radial folds, as a consequence of the parietal scarring.
A gastric peptic ulcer is a mucosal defect which penetrates the muscularis mucosae and lamina propria, produced by acid-pepsin aggression. Ulcer margins are perpendicular and present chronic gastritis. During the active phase, the base of the ulcer shows 4 zones: inflammatory exudate, fibrinoid necrosis, granulation tissue and fibrous tissue. The fibrous base of the ulcer may contain vessels with thickened wall or with thrombosis.[31]