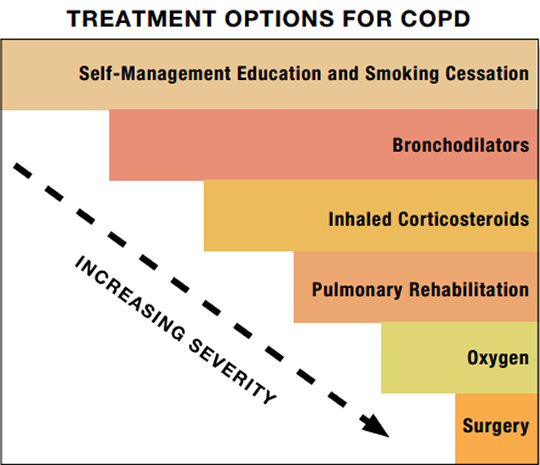
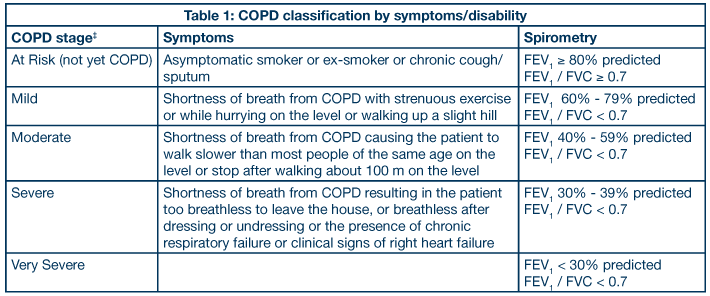
COPD has no cure yet. However, lifestyle changes and treatments can help you feel better, stay more active, and slow the progress of the disease.
The goals of COPD treatment include:
- Relieving your symptoms
- Slowing the progress of the disease
- Improving your exercise tolerance (your ability to stay active)
- Preventing and treating complications
- Improving your overall health
To assist with your treatment, your family doctor may advise you to see a pulmonologist. This is a doctor who specializes in treating lung disorders.
Lifestyle Changes
Quit Smoking and Avoid Lung Irritants
Quitting smoking is the most important step you can take to treat COPD. Talk with your doctor about programs and products that can help you quit.
If you have trouble quitting smoking on your own, consider joining a support group. Many hospitals, workplaces, and community groups offer classes to help people quit smoking. Ask your family members and friends to support you in your efforts to quit.
Also, try to avoid secondhand smoke and places with dust, fumes, or other toxic substances that you may inhale.
For more information about how to quit smoking, go to the Health Topics Smoking and Your Heart article and the National Heart, Lung, and Blood Institute's "Your Guide to a Healthy Heart." Although these resources focus on heart health, they include basic information about how to quit smoking.
Other Lifestyle Changes
If you have COPD, you may have trouble eating enough because of your symptoms, such as shortness of breath and fatigue. (This issue is more common with severe disease.)
As a result, you may not get all of the calories and nutrients you need, which can worsen your symptoms and raise your risk for infections.
Talk with your doctor about following an eating plan that will meet your nutritional needs. Your doctor may suggest eating smaller, more frequent meals; resting before eating; and taking vitamins or nutritional supplements.
Also, talk with your doctor about what types of activity are safe for you. You may find it hard to be active with your symptoms. However, physical activity can strengthen the muscles that help you breathe and improve your overall wellness.
Medicines
Bronchodilators
Bronchodilators relax the muscles around your airways. This helps open your airways and makes breathing easier.
Depending on the severity of your COPD, your doctor may prescribe short-acting or long-acting bronchodilators. Short-acting bronchodilators last about 4–6 hours and should be used only when needed. Long-acting bronchodilators last about 12 hours or more and are used every day.
Most bronchodilators are taken using a device called an inhaler. This device allows the medicine to go straight to your lungs. Not all inhalers are used the same way. Ask your health care team to show you the correct way to use your inhaler.
If your COPD is mild, your doctor may only prescribe a short-acting inhaled bronchodilator. In this case, you may use the medicine only when symptoms occur.
If your COPD is moderate or severe, your doctor may prescribe regular treatment with short- and long-acting bronchodilators.
Combination Bronchodilators Plus Inhaled Glucocorticosteroids (Steroids)
If your COPD is more severe, or if your symptoms flare up often, your doctor may prescribe a combination of medicines that includes a bronchodilator and an inhaled steroid. Steroids help reduce airway inflammation.
In general, using inhaled steroids alone is not a preferred treatment.
Your doctor may ask you to try inhaled steroids with the bronchodilator for a trial period of 6 weeks to 3 months to see whether the addition of the steroid helps relieve your breathing problems.
Vaccines
Flu Shots
The flu (influenza) can cause serious problems for people who have COPD. Flu shots can reduce your risk of getting the flu. Talk with your doctor about getting a yearly flu shot.
Pneumococcal Vaccine
This vaccine lowers your risk for pneumococcal pneumonia (NU-mo-KOK-al nu-MO-ne-ah) and its complications. People who have COPD are at higher risk for pneumonia than people who don't have COPD. Talk with your doctor about whether you should get this vaccine.
Pulmonary Rehabilitation
Pulmonary rehabilitation (rehab) is a broad program that helps improve the well-being of people who have chronic (ongoing) breathing problems.
Rehab may include an exercise program, disease management training, and nutritional and psychological counseling. The program's goal is to help you stay active and carry out your daily activities.
Your rehab team may include doctors, nurses, physical therapists, respiratory therapists, exercise specialists, and dietitians. These health professionals will create a program that meets your needs.
Oxygen Therapy
If you have severe COPD and low levels of oxygen in your blood, oxygen therapy can help you breathe better. For this treatment, you're given oxygen through nasal prongs or a mask.
You may need extra oxygen all the time or only at certain times. For some people who have severe COPD, using extra oxygen for most of the day can help them:
- Do tasks or activities, while having fewer symptoms
- Protect their hearts and other organs from damage
- Sleep more during the night and improve alertness during the day
- Live longer
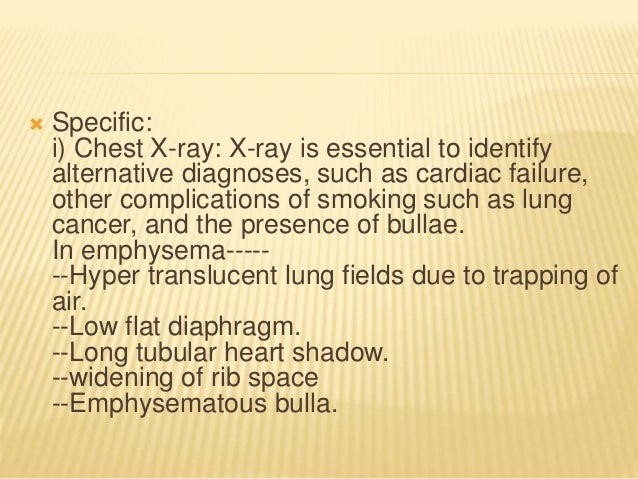
Surgery
Surgery may benefit some people who have COPD. Surgery usually is a last resort for people who have severe symptoms that have not improved from taking medicines.
Surgeries for people who have COPD that's mainly related to emphysema include bullectomy (bul-EK-toe-me) and lung volume reduction surgery (LVRS). A lung transplantmight be an option for people who have very severe COPD.
Bullectomy
When the walls of the air sacs are destroyed, larger air spaces called bullae (BUL-e) form. These air spaces can become so large that they interfere with breathing. In a bullectomy, doctors remove one or more very large bullae from the lungs.
Lung Volume Reduction Surgery
In LVRS, surgeons remove damaged tissue from the lungs. This helps the lungs work better. In carefully selected patients, LVRS can improve breathing and quality of life.
Lung Transplant
During a lung transplant, your damaged lung is removed and replaced with a healthy lung from a deceased donor.
A lung transplant can improve your lung function and quality of life. However, lung transplants have many risks, such as infections. The surgery can cause death if the body rejects the transplanted lung.
If you have very severe COPD, talk with your doctor about whether a lung transplant is an option. Ask your doctor about the benefits and risks of this type of surgery.